How can Digital Health be Implemented as envisaged in the National Health Policy 2017? by Prof. Supten Sarbadhikari @supten
It has been now more than a year that the (third edition of the) National Health Policy 2017 (NHP-2017) of India has been notified. While the accompanying Situation Analysis didn’t mention anything about Digital Health, the Policy correctly identified the need for creating many new institutions like the National Digital Health Authority (NDHA).
Now, let us look at where do we stand one year later, regarding the ushering in of Digital Health in India.
First let us glance at some of the key provisions of the NHP-2017 as mentioned in the various sections. Just beneath the quotes from the relevant sections of the NHP-2017, I’m commenting on certain issues for thought.
2.4.3.3 Health Management Information
a. Ensure district-level electronic database of information on health system components by 2020.
b. Strengthen the health surveillance system and establish registries for diseases of public health importance by 2020.
c. Establish federated integrated health information architecture, Health Information Exchanges and National Health Information Network by 2025.
Comments: The NHP-2017 focuses on Digital technology, right from the beginning. Some timelines are also proposed here. However, while some states have been doing very well, some others are lagging. We would further elaborate on this aspect towards the end.
3.3 Organization of Public Health Care Delivery:
For effectively handling medical disasters and health security, the policy recommends that the public healthcare system retain a certain excess capacity in terms of health infrastructure, human resources, and technology which can be mobilized in times of crisis.
In order to leverage the pluralistic health care legacy, the policy recommends mainstreaming the different health systems. This would involve increasing the validation, evidence and research of the different health care systems as a part of the common pool of knowledge. It would also involve providing access and informed choice to the patients, providing an enabling environment for practice of different systems of medicine, an enabling regulatory framework and encouraging cross referrals across these systems.
Comments: Here there is a need for more caution since the other streams of medicine – viz., Ayurveda, Yoga and Naturopathy, Siddha, Unani and Homeopathy, follow entirely different principles from those followed by modern medicine. Therefore, cross referrals may add to the complexity and confusion, ultimately harming the patient.
11.1 Medical Education:
The policy recognizes the need to revise the under graduate and post graduate medical curriculum keeping in view the changing needs, technology and the newer emerging disease trends.
Comments: There have been a lot of issues regarding the Medical Council of India and the National Board of Examinations in the past, followed by a proposed revamping through the National Medical Commission. Despite all the proposed changes, one of the essential features that is amiss is the incorporation of health informatics essentials in all branches of health professional education. Without doing that, a smooth adoption of digital health is extremely difficult.
11.8 Public Health Management Cadre:
The policy proposes creation of Public Health Management Cadre in all States based on public health or related disciplines, as an entry criteria.
Comments: In continuation of the previous section, health information management must be embedded as an integral part for health and hospital management. Health Informatics weds both health information technology and health information management. Scaling up, public health informatics combines health informatics and population demographics.
13.12: Health Information System:
The objective of an integrated health information system necessitates private sector participation in developing and linking systems into a common network/grid which can be accessed by both public and private healthcare providers. Collaboration with private sector consistent with Meta Data and Data Standards and Electronic Health Records would lead to developing a seamless health information system. The private sector could help in creation of registries of patients and in documenting diseases and health events.
Comments: Most of the times various health information systems don’t talk to each other and therefore there is a dire need of Standards for interoperability. I would discuss this issue in greater details this issue towards the end, where I would talk about the Clinical Establishments Act.
14.2: Regulation of Clinical Establishments:
A few States have adopted the Clinical Establishments Act 2010. Advocacy with the other States would be made for adoption of the Act. Grading of clinical establishments and active promotion and adoption of standard treatment guidelines would be one starting point. Protection of patient rights in clinical establishments (such as rights to information, access to medical records and reports, informed consent, second opinion, confidentiality and privacy) as key process standards, would be an important step. Policy recommends the setting up of a separate, empowered medical tribunal for speedy resolution to address disputes /complaints regarding standards of care, prices of services, negligence and unfair practices. Standard Regulatory framework for laboratories and imaging centers, specialized emerging services such as assisted reproductive techniques, surrogacy, stem cell banking, organ and tissue transplantation and Nano Medicine will be created as appropriate.
Comments: Discussed below separately.
14.5: Medical Devices Regulation:
The policy recommends strengthening regulation of medical devices and establishing a regulatory body for medical devices to unleash innovation and the entrepreneurial spirit for manufacture of medical device in India. The policy supports harmonization of domestic regulatory standards with international standards. Building capacities in line with international practices in our regulatory personnel and institutions, would have the highest priority. Post market surveillance program for drugs, blood products and medical devices shall be strengthened to ensure high degree of reliability and to prevent adverse outcomes due to low quality and/or refurbished devices/health products.
Comments: Medical Devices Rules, 2017 that has come into force with effect from 1st day of January, 2018, has included in the Part-I of the first schedule Parameters for classification of medical devices other than in vitro diagnostic medical devices. There, Software as Medical Device (SaMD) is defined as: (iii) Software, which drives a device or influences the use of a device, falls automatically in the same class. This is indeed a very forward looking and welcome legislation, ahead of the times in our country.
22: Health Technology Assessment:
Health Technology assessment is required to ensure that technology choice is participatory and is guided by considerations of scientific evidence, safety, consideration on cost effectiveness and social values. The National Health Policy commits to the development of institutional framework and capacity for Health Technology Assessment and adoption.
Comments: We can combine these aspects with the digital health technology, described in the next section.
23: Digital Health Technology Eco – System:
Recognising the integral role of technology(eHealth, mHealth, Cloud, Internet of things, wearables, etc) in the healthcare delivery, a National Digital Health Authority (NDHA) will be set up to regulate, develop and deploy digital health across the continuum of care. The policy advocates extensive deployment of digital tools for improving the efficiency and outcome of the healthcare system. The policy aims at an integrated health information system which serves the needs of all stake-holders and improves efficiency, transparency, and citizen experience. Delivery of better health outcomes in terms of access, quality, affordability, lowering of disease burden and efficient monitoring of health entitlements to citizens, is the goal. Establishing federated national health information architecture, to roll-out and link systems across public and private health providers at State and national levels consistent with Metadata and Data Standards (MDDS) & Electronic Health Record (EHR), will be supported by this policy. The policy suggests exploring the use of “Aadhaar” (Unique ID) for identification. Creation of registries (i.e. patients, provider, service, diseases, document and event) for enhanced public health/big data analytics, creation of health information exchange platform and national health information network, use of National Optical Fibre Network, use of smartphones/tablets for capturing real time data, are key strategies of the National Health Information Architecture.
23.1 Application of Digital Health:
The policy advocates scaling of various initiatives in the area of tele-consultation which will entail linking tertiary care institutions (medical colleges) to District and Sub-district hospitals which provide secondary care facilities, for the purpose of specialist consultations. The policy will promote utilization of National Knowledge Network for Tele-education, Tele-CME, Tele-consultations and access to digital library.
23.2 Leveraging Digital Tools for AYUSH:
Digital tools would be used for generation and sharing of information about AYUSH services and AYUSH practitioners, for traditional community level healthcare providers and for household level preventive, promotive and curative practices.
Comments: This is a very correct decision and the first job for the proposed NDHA will be to formulate a robust National Digital Health Strategy / Policy, in consultation with all the stakeholders. The first constituents of the Authority will lay down the rules of the game as to how will digital health be adopted in India. The earlier the NDHA is set up and functional, the better it will be for India to avoid a digital health mess in future. Any delay in the process might make us deal with non-interoperable legacy systems, as has been the case in many developed nations. However, cross referrals and sharing disparate information among different systems of medicine may add to the complexity and confusion, ultimately harming the patient. Currently, the MoHFW is seeking comments on the proposed DISHA (Digital Information Security in Healthcare Act) that will be the Bill setting up the NDHA / NeHA.
25. Health Research:
The National Health Policy recognizes the key role that health research plays in the development of a nation’s health. In knowledge based sector like health, where advances happen daily, it is important to increase investment in health research.
25.1 Strengthening Knowledge for Health:
The policy envisages strengthening the publicly funded health research institutes under the Department of Health Research, the apex public health institutions under the Department of Health & Family Welfare, as well as those in the Government and private medical colleges. The policy supports strengthening health research in India in the following fronts- health systems and services research, medical product innovation (including point of care diagnostics and related technologies and internet of things) and fundamental research in all areas relevant to health- such as Physiology, Biochemistry, Pharmacology, Microbiology, Pathology, Molecular Sciences and Cell Sciences. Policy aims to promote innovation, discovery and translational research on drugs in AUSH and allocate adequate funds towards it. Research on social determinants of health along with neglected health issues such as disability and transgender health will be promoted. For drug and devices discovery and innovation, both from Allopathy and traditional medicines systems would be supported. Creation of a Common Sector Innovation Council for the Health Ministry that brings together various regulatory bodies for drug research, the Department of Pharmaceuticals, the Department of Biotechnology, the Department of Industrial Policy and Promotion, the Department of Science and Technology, etc. would be desirable. Innovative strategies of public financing and careful leveraging of public procurement can help generate the sort of innovations that are required for Indian public health priorities. Drug research on critical diseases such as TB, HIV/AIDS, and Malaria may be incentivized, to address them on priority. For making full use of all research capacity in the nation, grant- in- aid mechanisms which provide extramural funding to research efforts is envisaged to be scaled up.
25.2 Drug Innovation & Discovery:
Government policy would be to both stimulate innovation and new drug discovery as required, to meet health needs as well as ensure that new drugs discovered and brought into the market are affordable to those who need them most. Similar policies are required for discovering more affordable, more frugal and appropriate point of care diagnostics as also robust medical equipment for use in our rural and remote areas. Public procurement policies and public investment in priority research areas with greater coordination and convergence between drug research institutions, drug manufacturers and premier medical institutions must also be aligned to drug discovery.
25.3 Development of Information Databases:
There is also a need to develop information data-bases on a wide variety of areas that researchers can share. This includes ensuring that all unit data of major publicly funded surveys related to health, are available in public domain in a research friendly format.
25.4 Research Collaboration:
The policy on international health and health diplomacy should leverage India’s strength in cost effective innovations in the areas of pharmaceuticals, medical devices, health care delivery and information technology. Additionally leveraging international cooperation, especially involving nations of the Global South, to build domestic institutional capacity in green-field innovation and for knowledge and skill generation could be explored.
Comments: For health research and innovation the government’s role of encouraging Standards for interoperability and allowing open data for analysis will go a long way.
Apart from the NHP-2017, there are certain existing legislations that affects the adoption of digital health in India. The first and foremost is the 2012 Amendments of the Clinical Establishments Act 2010. The other guidance comes from the Constitution of India. Both of these are discussed below.
Clinical Establishments (Registration and Regulation) Act (CEA):
In 2012, the MoHFW amended the CEA (2010) and added Clause “9 (iv): the clinical establishments shall maintain and provide Electronic Medical Records (EMR) or Electronic Health Records (EHR) of every patient as may be determined and issued by the Central Government or the State Government as the case may be, from time to time”.
Comments: The Act has taken effect in the four states namely, Arunachal Pradesh, Himachal Pradesh, Mizoram, Sikkim, and all Union Territories since 1st March, 2012 vide Gazette notification dated 28th February, 2012. The states of Uttar Pradesh, Uttarakhand, Rajasthan, Jharkhand, Bihar and Assam have adopted the Act under clause (1) of article 252 of the Constitution.
The Ministry has notified the National Council for Clinical Establishments and the Clinical Establishments (Central Government) Rules, 2012 under this Act vide Gazette notifications dated 19th March, 2012 and 23rd May, 2012 respectively.
The Act is applicable to all kinds of clinical establishments from the public and private sectors, of all recognized systems of medicine including single doctor clinics. The only exception will be establishments run by the Armed forces.
The good point is the enactment of the necessity for EMR / EHR. The Ministry of Health and Family Welfare has been notifying Standards for EHR since August 2013 and the second edition of the Guidelines were notified in December 2016. That is the right way to move forward. However, Health being a State subject, not all the states are equally keen to adopt it.
Concurrent List: The seventh schedule of the Constitution of India lists “Health” (Public health and sanitation; hospitals and dispensaries) under the Item 6 of List-II (State list). As expected, like the Union ministry, health ministers of various states have also agreed to equipping PHCs and CHCs with latest technology.
Comments: However, as seen in the previous section, the CEA has not yet been adopted by most of the states of India. Therefore, although the CEA mandates EMR / EHR, most of the states are not yet bound to follow it. Since Health is neither in the Union list, nor in the Concurrent list, it may be prudent to include it in the Concurrent list. In that case adoption of digital health would be much smoother.
Conclusions:
While the NHP-2017 is bold in its thoughts and foresight, for facilitating digital health, the ground realities don’t appear to have been considered well enough. Early setting up of a functional NDHA is essential for India to avoid a digital health mess in future. Inordinate delays might make us deal with non-interoperable legacy systems. The first job for the proposed NDHA will be to formulate a robust National Digital Health Strategy / Policy, in consultation with all the stakeholders.
Caution needs to be exercised before cross referrals and sharing disparate information among different systems of medicine. Health informatics education must be embedded as an integral part for health and hospital management. Since Health is neither in the Union list, nor in the Concurrent list of the Constitution of India, it may be prudent to include it in the Concurrent list. In that case adoption of digital health would be much smoother.
Seeking comments on the Draft Bill DISHA (Digital Information Security in Healthcare Act) is a good start.
References:
[1]: Ministry of Health and Family Welfare, Government of India, National Health Policy 2017: https://www.nhp.gov.in//NHPfiles/national_health_policy_2017.pdf (Accessed 19th February 2018)
[2]: Ministry of Health and Family Welfare, Government of India. Situation Analyses: Backdrop to the National Health Policy – 2017, New Delhi. Available from : https://mohfw.gov.in/sites/default/files/71275472221489753307.pdf
[3]: Sundararaman T, National Health Policy 2017: A Cautions Welcome, Indian J Med Ethics. 2017 Apr-Jun;2(2):69-71
[4]: Sarbadhikari SN. A farce called the National Board of Examinations. Indian J Med Ethics. 2010 Jan-Mar;7(1):20-2
[5]: Thomas G, Medical education in India – the way forward, Indian J Med Ethics. 2016 Oct-Dec;1(4):200
[6]: Government of India, The Gazette of India, dated 31/01/2017: http://www.cdsco.nic.in/writereaddata/Medical%20Device%20Rule%20gsr78E(1).pdf (Accessed 19th February 2018)
[7]: Government of India, The Gazette of India, dated 19/8/2010, Clinical Establishments (Registration and Regulation) Act 2010:
http://clinicalestablishments.nic.in/WriteReadData/969.pdf (Accessed 19th February 2018)
[8]: Government of India, The Gazette of India, dated 23/5/2012, Clinical Establishments (Registration and Regulation) Act, (Amendments) 2012:
http://clinicalestablishments.nic.in/WriteReadData/386.pdf (Accessed 19th February 2018)
[9]: Ministry of Health and Family Welfare, Government of India. http://clinicalestablishmentstraining.nic.in/cms/Home.aspx (Accessed 19th February 2018)
[10]: National Health Portal, Ministry of Health and Family Welfare, Government of India, EHR Standards: https://www.nhp.gov.in/electronic-health-record-standards-for-india-helpdesk_mty (Accessed 19th February 2018)
[11]: Government of India, The Constitution of India http://lawmin.nic.in/olwing/coi/coi-english/coi-4March2016.pdf (Accessed 19th February 2018)
[12]: Press Information Bureau, Government of India, Shri J P Nadda chairs 12th Conference of the Central Council of Health and Family Welfare to discuss Draft National Health Policy, dated 27/02/2016: http://pib.nic.in/newsite/PrintRelease.aspx?relid=136961 (Accessed 19th February 2018)
[13]: Ministry of Health and Family Welfare, Government of India. https://mohfw.gov.in/newshighlights/comments-draft-digital-information-security-health-care-actdisha (Accessed 28th March 2018)
[14]: National Health Portal, Ministry of Health and Family Welfare, Government of India, EHR Standards: https://www.nhp.gov.in/ehr-standards-helpdesk_ms (Accessed 28th March 2018)
The article was first published on Dr. Supten’s Blog here, its been re-published here with the author’s permission.
[tab]
[content title=”About Prof. Supten Sarbadhikari”]
[/content]
[content title=”Latest Articles”]
[/content] [/tab]













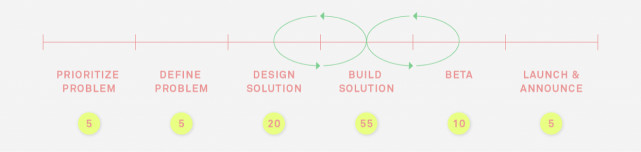
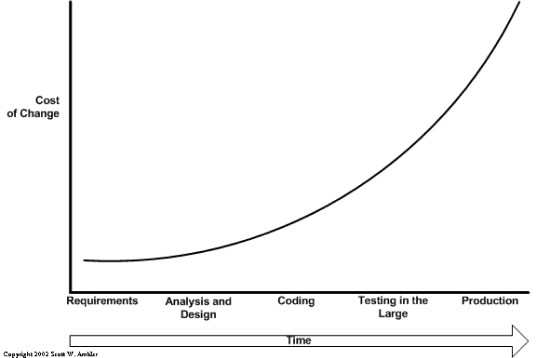
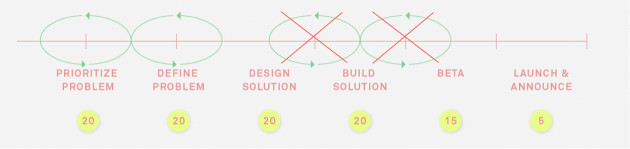

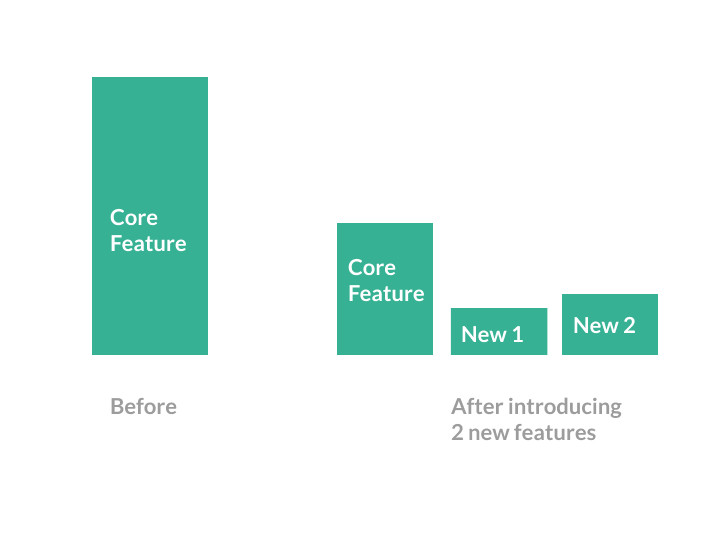 How can you solve your metrics problems then? Well, small incremental efforts towards optimising your AARRR funnels will help you improve your pirate metrics not always a new feature.
How can you solve your metrics problems then? Well, small incremental efforts towards optimising your AARRR funnels will help you improve your pirate metrics not always a new feature.





You must be logged in to post a comment.